
Health Blog | 3 MIN READ
Iliotibial Band (ITB) Syndrome
Dr. Katherine Valdez
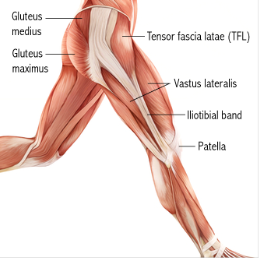
Iliotibial Band is a thick fibrous band on the lateral side of the knee, that runs from the outside of the pelvis, over the hip and knee, and inserted just below the knee. It is a long fibrous reinforcement of the fascia lata that is associated in different muscle movement such flexion, extension, abduction and lateral rotation of the hip. The band is crucial in stabilizing the knee and knee’s main support against gravity.
Causes


Iliotibial Band Syndrome is the second most common knee injury, it is usually caused by friction between the ITB and lateral femoral epicondyle that leads to the irritation or swelling of the lateral knee, which is mostly seen in runner, cyclist, hikers or new gym goers. It is also caused by overuse and repetitive flexion and extension movement of the knee and it can be also caused by a poor physical condition, lack of warming up before exercise, drastic change in activity level or wearing improper footwear.
Symptoms and Risk
ITB Syndrome symptoms range from stinging sensation on the lateral side of the knee, to swelling or tenderness upon palpation to thickening of the tissue on the area where the band moves that causes limitation or tightness of the movement.
The pain and limitation can also vary depending on the onset and location of pain. The pain over the knee may not be felt immediately during the activity, but may intensify over time. Pain felt when the heel touches the ground might persist after the activity. Pain may also be present above or below the knee, where the band attaches.
But if you are not an athlete, ITB syndrome can also be seen in individuals that have bowed legs, uneven leg length, someone with knee arthritis or someone with weakness of the hip, butt, or abdominal muscle. These individuals are at risk of having ITB syndrome if those issues are not addressed properly.
Diagnosis
To rule in whether an individual have ITB syndrome, upon physical examination and patient interview, the doctor will ask about the location and onset of pain and the patient’s daily activities or lifestyle. One of the tests to perform in ruling in ITB syndrome is called Ober Test’s.

1. Ober's Test
Ober’s Test evaluates a tight, contracted, or inflamed tensor fascia Lata muscle and iliotibial band. It requires the patient to side lie on the opposite side of the tested side, where the tested limb is facing upwards. The doctor will guide the affected leg backwards and gently drops it down towards the bed. If the tested leg has a difficulty on bringing it close to the bed, that means it is positive of the test ruling in ITB syndrome.
To differentiate it from other knee pain and injuries, the doctor might request for detailed imaging or perform few tests to rule it out like Patellar Grind Test or Clarke’s Test for Patellofemoral Pain Syndrome also known as runner’s or jumper’s knee.
2. Patellar Grind Test
Patellar Grind Test, also known as Clarke’s Test, is used to assess the reason for knee pain, where the patient is positioned in a supine or long sitting with the tested leg in extension. The doctor will place his or her web space above the kneecap while applying pressure, then instruct the patient to slowly contract his or her quads. If the patient felt pain behind his or her knee cap while contracting the quads, means the test is positive.

Treatment
Now that we’ve rule in and certain about ITB syndrome, the treatment plan may vary based on the severity of symptoms. Many non-surgical treatments are helpful in treating ITB syndrome, here are commonly recommended treatment to decrease the pain and tension on the ITB.
• Rest. Individuals with ITB syndrome may need to decrease the intensity, duration, and frequency of activity. It may be upsetting for an active individual to cut or decrease their physical activity but it is necessary to provide a healing period for the injury.
• Medications. Individuals with ITB syndrome may need to decrease the intensity, duration, and frequency of activity. It may be upsetting for active individuals to cut or decrease their physical activity but it is necessary to provide healing period for the injury.
• Physiotherapy. A physiotherapist can perform manual therapy such as deep tissue release, mobilization and stretching to decrease the tension and tightness over the lateral side of the knee and provide pain relief. The physiotherapist will also provide stabilization and strengthening exercises for postural correction and maintaining a good structural form of the knee to prevent the injury from reoccurring.
In some chronic cases where conservative treatments don’t work, surgical treatment is recommended. ITB Surgical Release is an invasive procedure where a small incision is done on the lateral side of the knee and removes a small portion of the iliotibial band that has contact on the thighbone (lateral femoral epicondyle). The complete recovery from the surgery usually takes 4 to 6 weeks, with one week after the surgery, the patient can perform daily activities without the use of crutches.
Exercises
1. Stretching Exercises for 30 sec holds for 3 reps
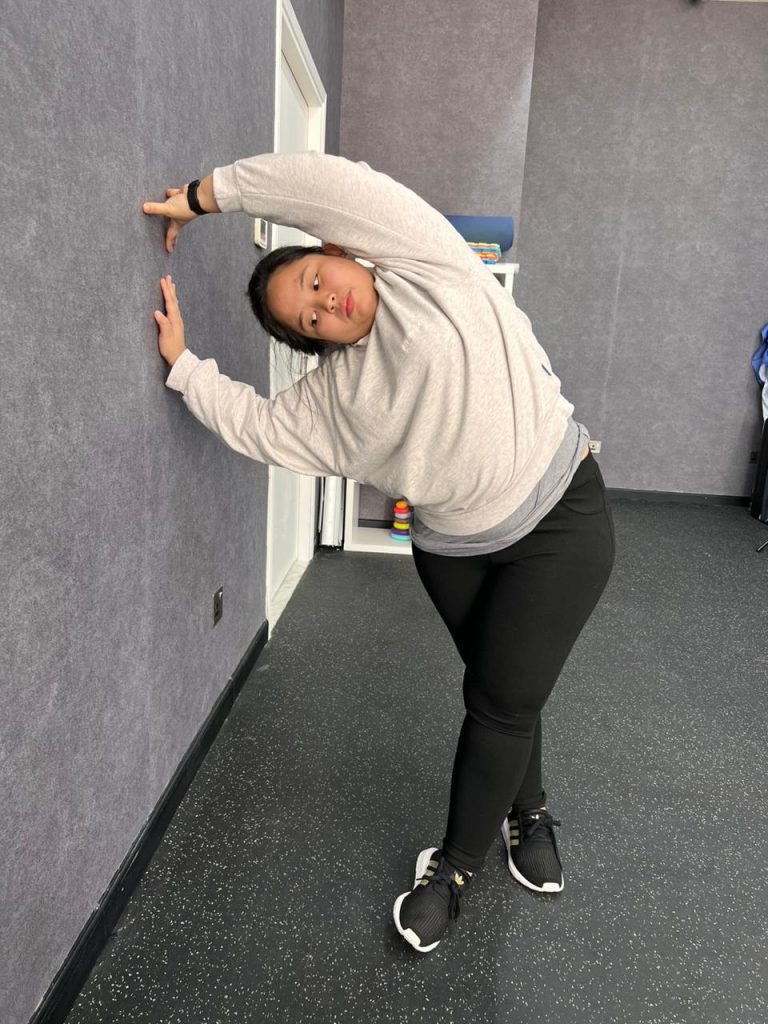
a. ITB stretch. The patient will stand beside the wall, where the affected leg is away from the wall. The patient then crosses the affected leg forward to the unaffected leg, then the patient will try to reach the wall on the side.
b. Quads stretch. In standing, the patient will stand on the unaffected leg while grabbing the affected leg from behind. The patient can hold in a chair for support.


c. Hamstring stretch. In the supine position, they are asked to elevate their leg using a band or towel while maintaining their knees straight.


2. Strengthening Exercises for 10 reps with 2 – 3 sets
a. VMO Activation. The patient will be asked to perform a squat but with a ball or pillow in between the legs. While performing the squats, the patient will simultaneously squeeze the ball and hold for 7 sec before standing up.


b. Pelvic Bridging with bands. In the supine position, the patient will bend both her knees and place the band between her legs. Then the patient will be asked to lift his pelvis up while simultaneously trying to abduct his or her legs.


c. Side - lying Leg Lifts. In the side-lying position, the patient will place a band around the ankle area and will lift his or her leg up.


d. Clamshell Exercise. In the side-lying position, the patient will bend his or her knees with ankles touching each other, then patient will lift his or her leg without separating the ankle from each other.



e. Knee Stabilization. In the standing position, the patient will place a band on his ankle while the other side of the band is tied in a pole, then the patient will perform all hip motions (flexion, extension, abduction and adduction)




